TMS Side Effects
~ 2 Minute Read
By Mhd Khaled Bowarshi, M.D.
TMS Psychiatrist at Florida TMS Clinic
Before starting
TMS Therapy, you must know the risks that could be associated with TMS. Obviously, just like anything in medicine, every treatment has its own benefits and risks. Knowing the
pros and cons of TMS should help you make a better decision about choosing TMS over other depression treatment options. In this article, we will discuss the absolute contraindications of TMS, relative contraindications of TMS and then the side effects of TMS. You will notice that TMS is for the most part doesn't have systemic side effects. TMS side effects are local like local scalp discomfort at the site of the TMS coil placement.
What are the absolute contraindications for TMS?
The main absolute contraindication for TMS therapy is the presence of a movable ferromagnetic intracranially (inside the head). In other words, if someone has a brain stent, clip, or stimulator then this person should not be receiving TMS therapy. There are other relative contraindications for TMS that will require further evaluation with the doctor before TMS therapy.
What are the relative contraindications for TMS?
The list of contraindications includes a history of seizure, head injury, brain surgery, any metal in the head (outside of the skull) such as shrapnel, surgical clips, or fragments. Implanted devices such as pacemakers. The presence of any of the above warrants further investigation and discussion with the doctor to evaluate the benefits vs the risks of TMS therapy.
Is Transcranial Magnetic Stimulation safe?
For the right patient, the answer is; Yes. TMS is one of the safest treatments currently available for depression aside from talk therapy. TMS therapy has proven safety and efficacy in many clinical trials.
What are the negative side effects of TMS Therapy?
The most common side effect of TMS therapy is scalp irritation or discomfort. It is reported in about 5% of patients and it usually goes away after a few sessions. The other side effects of TMS is seizure, which is very rare.
Can TMS therapy cause seizures?
Yes. Though it is very rare, TMS therapy can induce a seizure. It is estimated to happen in 1/30,000 treatments. Considering that each patient is getting about 30 sessions. This is estimated to happen at a rate of 0.1%. That chance is one in a thousand. To put this in perspective, one of the antidepressants; Wellbutrin is estimated to cause seizures in 0.4% which is four in a thousand. In other words, some medications have more risk to induce seizures than TMS. That being said, every patient undergoing TMS therapy should have a full evaluation by a TMS psychiatrist to screen for medical issues and current medications that could alter the risk of seizures.
Is Transcranial Magnetic Stimulation painful? Does TMS hurt?
For most patients, the answer is; No. TMS doesn’t hurt for the vast majority of people. Pain is subjective. About 5% of patients treated with TMS report head discomfort in the first 4-5 sessions. It mostly goes away as they get used to the treatment. A very small minority of patients could experience a tension headache. This usually goes away in 30 minutes to 2 hours. In some cases, Tylenol or Ibuprofen can be helpful. It can be avoided by starting the magnetic stimulation intensity low and increasing gradually.
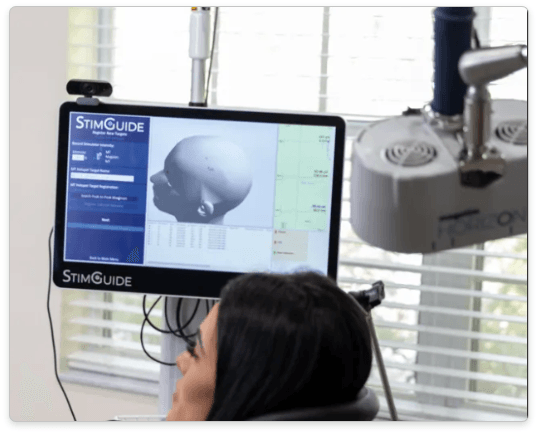
What does Transcranial Magnetic Stimulation feel like?
It simply feels like a woodpecker on the side of the head. As the patient is basically laying in a spa-like chair watching Netflix, most of the time this feeling disappears in the background after a few minutes.
Does TMS Therapy cause Migraine?
TMS could cause mild head discomfort in about 5% of patients. Rarely some patients could experience a headache. It is usually more of a tension-type of headache, not a migraine headache. Also, there is a single pulse TMS device that is actually FDA-cleared for migraine headache treatment. See the section for TMS Therapy Uses above.
Does TMS Therapy cause hearing loss?
Constant exposure to loud noise could cause some hearing damage. It is highly recommended that patients wear earplugs during their TMS sessions to avoid hearing loss. In fact, we ask all of our patients to do so. Earplugs decrease the level of noise by about 30 dB which puts it in the safe range.
Does TMS Therapy cause brain damage?
No. TMS doesn’t cause brain damage. This is assuming that all the screening measures are taken and there are no contraindications to the magnetic treatment (no ferromagnetic metals in the brain).
Does TMS Therapy cause memory loss?
There is no clinical evidence that TMS causes memory loss. On the other hand, there is clinical evidence to the contrary. TMS could actually enhance memory and cognition. Many researchers are looking into the use of TMS for cognitive enhancement and treatment of early dementia.
Does TMS Therapy cause insomnia?
Not directly. On the contrary, many patients report improvement in sleep after a few sessions. There are trials looking into using TMS for insomnia.
Does TMS Therapy cause lucid dreams?
Possibly. Some patients report lucid dreams especially in the first week of treatment. We don’t have reports of nightmares though.
Can TMS Therapy be done with dental implants?
Yes. For the vast majority of cases, TMS therapy can be performed with dental implants. Please share with your TMS doctor where and what dental implants you have to discuss more and monitor.
Can TMS Therapy be done with a heart pacemaker?
Possibly, but with extra care, TMS can be done with a cardiac pacemaker. It requires very detailed evaluation. Coordination with the cardiologist and electrophysiologist to make sure the pacer and battery interrogated recently. We also would need to contact the manufacturer (Medtronic for example), depending on the model, they might recommend and send us a "shield".
Can TMS Therapy be done with a brain stimulator?
No. TMS is contraindicated with a brain pacemaker (deep brain stimulator). Brain pacemakers are used for deep brain stimulation in some cases of refractory Parkinson’s disease and respiratory depression.
Can you have TMS Therapy if you have a Spinal Cord Stimulator?
Yes, one can have TMS with a spinal stimulator. Assuming the stimulator in the thoracic or lumbar spine.
References:
O'Reardon JP, Solvason HB, Janicak PG, Sampson S, Isenberg KE, Nahas Z, McDonald WM, Avery D, Fitzgerald PB, Loo C, Demitrack MA, George MS, Sackeim HA. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial. Biol Psychiatry. 2007 Dec 1;62(11):1208-16. doi: 10.1016/j.biopsych.2007.01.018. Epub 2007 Jun 14. PMID: 17573044.
Perera T, George MS, Grammer G, Janicak PG, Pascual-Leone A, Wirecki TS. The Clinical TMS Society Consensus Review and Treatment Recommendations for TMS Therapy for Major Depressive Disorder. Brain Stimul. 2016 May-Jun;9(3):336-346. doi: 10.1016/j.brs.2016.03.010. Epub 2016 Mar 16. PMID: 27090022; PMCID: PMC5612370.
McClintock SM, Reti IM, Carpenter LL, McDonald WM, Dubin M, Taylor SF, Cook IA, O'Reardon J, Husain MM, Wall C, Krystal AD, Sampson SM, Morales O, Nelson BG, Latoussakis V, George MS, Lisanby SH; National Network of Depression Centers rTMS Task Group; American Psychiatric Association Council on Research Task Force on Novel Biomarkers and Treatments.
Consensus Recommendations for the Clinical Application of Repetitive Transcranial Magnetic Stimulation (rTMS) in the Treatment of Depression. J Clin Psychiatry. 2018 Jan/Feb;79(1):16cs10905. doi: 10.4088/JCP.16cs10905. PMID: 28541649; PMCID: PMC5846193.